Researchers at Cinvestav in Mexico have produced a promising vaccine candidate against Alzheimer’s disease by targeting the amyloid-beta (Aβ) peptide. The vaccine, created by a team led by Miguel Angel Gómez Lin, used an Aβ epitope – a molecule-specific receptor – that is known to be present in the full-length amyloid-beta peptide, as well as in its truncated version, which is often found in the brains of Alzheimer’s patients. After immunization, Aβ-specific antibodies from the mice were isolated and found to effectively bind to amyloid plaques in both mice and human brains (Inflammopharmacol doi: 10.1007/s10787-017-0408-2).
Designing the best vaccine
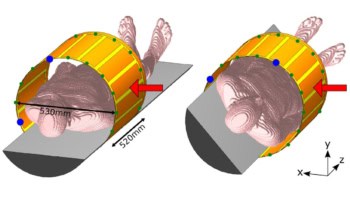
Virus-like particles (VLPs) are an exciting approach to vaccines because of their natural immunogenic properties. They also have an improved safety profile compared with vaccines based on live or attenuated virus. VLPs self-assemble from many copies of a protein and can present antigens on their surface at high density. Lim’s team decided to use the HPV (human-papilloma virus) VLP: a well-characterized platform that is able to support the genetic insertion of foreign epitopes.
After constructing three-dimensional molecular models of the assembled VLP (formed from 72 pentameric HPV protein shells), the researchers found two promising areas to insert their Aβ epitope. Choosing the place for genetic insertion on a VLP is not trivial since the inserted epitope needs to both face the outside of the nanocage to facilitate binding and not interfere with VLP formation.
The team chose the epitope inserted in the VLP (epitope Aβ 11-28) because it is present in both full-length amyloid-beta peptide and in the truncated/modified versions of peptides that are pathogenic. Although there are different proposed mechanisms of Alzheimer’s disease, the amyloid peptide is hypothesized to cause toxicity in the brain by forming large, insoluble plaques between neurons.
A promising proof-of-principle
After producing the VLP vaccine in plants, the researchers assessed the vaccine by immunizing mice. They tested samples from the mice for the presence of anti-amyloid-β antibodies at the end of a 10-week immunization period.
The results speak for themselves: not only did the mice serum contain antibodies that were able to recognize both the full-length and truncated amyloid peptide, but the antibodies were also able to bind to amyloid plaques in Alzheimer’s disease brain samples from mice and humans.
Taken together, these results are an important step towards creating an immunogenic therapy for Alzheimer’s disease. The VLP-based vaccine developed by the Mexico-based research centre was not only safe and easy to produce, but also showed good immunogenicity and the ability to target different amyloid peptides and amyloid aggregates.
Although no vaccine against Alzheimer’s exists yet, research results like this hopefully bring us one step closer.