CT imaging is ubiquitous in lung cancer management – with scans employed for diagnosis, radiotherapy set-up and response assessment. But according to Iain Phillips from Royal Surrey County Hospital, the information contained within a standard CT scan could be used for a lot more.
Speaking at the recent MediSens conference in London, Phillips described how texture analysis of lung CT scans could be used to identify whether a lung cancer patient is fit enough to undergo radiotherapy. “Texture analysis is based on the idea that imaging provides a pool of unmined data, and that we can get more technical information from a standard image and greater value from fewer tests,” he explained.
Lung cancer patients often have multiple morbidities, such as chronic obstructive pulmonary disease, for example, which causes breathing difficulties. As a lower post-operative lung function increases mortality, patients scheduled for surgical lung cancer treatment are classified as fit or unfit for surgery beforehand, using simple tests such as spirometry.
Spirometry assesses lung function by measuring how much air a patient can breathe out in one forced breath (FEV1, the forced expiratory volume in one second). Physicians also assess the transfer factor TLCO, which measure’s the lung’s ability to transfer oxygen into tissue.
When considering surgery, a patient with an estimated post-operative TLCO or FEV1 of below 40% predicted is considered at high risk. But for radiotherapy, there are no standard thresholds in use and no model that describes the impact of lung function on radiotherapy side-effects. It is likely, however, that a lower lung function will lead to more adverse effects.
Texture mapping
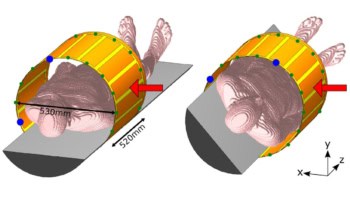
To investigate the use of CT scans for assessing patient fitness, Phillips and colleagues devised an analysis methodology. Using a cylinder of lung tissue, they perform a voxel-by-voxel analysis to create a texture map of this region-of-interest (ROI). Each voxel is assigned a density value and an entropy score. The entropy score is based on the similarity of grey levels in adjacent voxels, with a high entropy describing a low uniformity, and vice versa.
Phillips described a texture analysis and lung function study of 30 fit and 30 unfit patients who had undergone radical radiotherapy (chemo-radiotherapy or stereotactic ablative radiotherapy). Patients were defined as fit if they had FEV1 and TLCO values of 50% predicted or higher; if either parameter was below 50% the patient was classified as unfit. The researchers used the patients’ 4DCT scans to perform a retrospective imaging review, calculating the mean, median and mode values of density and entropy.
Looking at the texture maps created from the CT scans, maps from fit patients included more white (heterogenous) regions, whilst maps from unfit patients had more black (homogeneous) regions. This homogeneity is likely due to emphysema, the presence of holes in the lung tissue, as seen in less well functioning lungs. Plots of density versus entropy for the two patient groups clearly revealed different regions of data cluster.
The study concluded that patients with good lung function exhibit texture maps with voxels of higher entropy and higher density, whilst poorer lung function corresponds to lower entropy and lower density. “It appears to be possible to differentiate between fit and unfit patients just by looking at the CT image, and getting functional data from the CT scan,” said Phillips.
To use this technique clinically, Phillips suggests a “simple ROI” scheme, in which the ROI is identified automatically following CT acquisition, then texture analysis is performed, and only at this stage is the clinician required to review the results. “This offers a simple way of including advanced image analysis into the normal radiology workflow,” he explained.
Phillips suggests that this CT-based approach could be used as a screening test for both surgery or radiotherapy, enabling faster decision-making at multidisciplinary team meetings. It could also play a role in resource-limited settings. “In terms of use in clinical practice, we can start applying this to patients, to assess whether they are fit for treatments,” Phillips concluded.